
A Season in Hell
By Mark Dery
On the wall at the foot of my bed, a poster displays the Faces Pain Scale, a series of earless, genderless everymen arranged, from right to left, in increasing degrees of agony.1

“The faces show how much pain or discomfort someone is feeling,” the caption explains. “The face on the left shows no pain. Each face shows more and more pain and the last face shows the worst pain possible. Point to the face that shows how bad your pain is right NOW.”2 The blurb adds, helpfully, that your face need not resemble the cartoon visages in the Pain Scale.
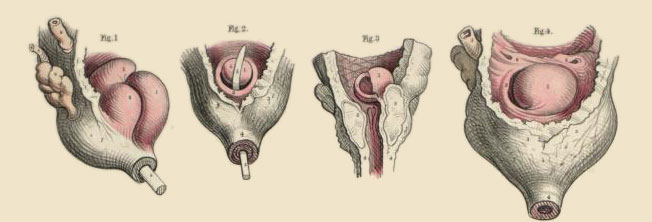
It’s August 2011. I’m lying in a room at New York-Presbyterian Hospital, waiting to undergo surgery for a small-bowel obstruction, an intestinal blockage resulting from postoperative adhesions caused by my 2008 surgery for my first small-bowel obstruction, itself the result of my 2006 surgery for a rare and virulent cancer. Abdominal surgery begets scar tissue. Which gives rise to adhesions. Which sometimes cause bowel obstructions. Which may necessitate surgery. Which begets more scar tissue, which…
I’m feeling nigh unto death, driven half-mad by my nasogastric tube, a tube running up my nose and down my throat, pumping a bilious green froth of stomach acid and half-digested goop out of my belly, into the canister behind my headboard.
(Few readers will know firsthand the horror of the NG tube, or, more exactly, of its insertion. Handing you a cup of water, the doctor prods a plastic tube up one of your nasal passages, down your throat and into your stomach, exhorting you to drink, drink, DRINK! to ease the tube’s passage and suppress your gag reflex. The violation is over in seconds, but for those seconds the retching, suffocating nightmare is unendurably awful, like drowning on dry land. And for the days or weeks that the tube lives in you, like some parasitoid alien organism, you gag a little every time you swallow, the tube rasping against your throat.)
In my agony, I take some small comfort in knowing that the Faces Pain Scale is there for me, even if I don’t look like a constipated mime.

In 2006, I was diagnosed with squamous-cell cancer of the urethra, a rare form of the disease. I spent that summer at the Memorial Sloan-Kettering Cancer Center, riding the sickening swells of a chemotherapy so toxic it left me limp and nauseous for the first of the two weeks between each session, poisoned by the cure that felt as if it was killing me.
By summer’s end, it had shrunk my tumor, but not enough. Thus, my date with the O.R. at New York-Presbyterian—foreordained from the moment my surgeon saw my first MRI—would be more harrowing than I’d hoped. “Of course, it was dispiriting,” I told my friends, in one of the periodic e-mail updates I called cancer-grams. “I had hoped that the tumor would shrivel up and die, nuked by the chemo.” That said, I noted,
The most painful part of having my hopes dashed was the deadpan affect with which my Sloan-Kettering oncologist delivered the news that my chemo had failed, adding that, in his considered opinion, I should have my everything removed as an offering to the Angry God of Cancer, in the desperate hope that this thing will never come back. “Radical penectomy,” he snapped, tonelessly. Then, without so much as a handshake, he swept out of the room, white coat flapping. That, I gathered, was the end of our doctor-patient relationship.
I’ll always remember him as a man who put the “care” in “caregiver,” with a bedside manner whose saintly compassion and twinkly-eyed avuncularity recalled Joseph Mengele at his best.3
Mercifully, my surgeon was as profoundly humane as my Sloan-Kettering doctor was bloodless. Dr. James McKiernan struck a delicate balance between an unfeigned compassion, leavened with a hilariously bent wit, and an unassuming mastery of his field. He was by all accounts preternaturally skilled with a scalpel. A radical penectomy, he reassured me with an eyeroll, would not be necessary.
In October 2006, Dr. McKiernan carved away my cancer in an epic operation. Since then, I’ve undergone MRIs and CAT scans at ever-greater intervals. So far, no bogeys have appeared on the radar screen; hitting the five-year mark without incident, as I have, means that the statistical likelihood of a recurrence is astronomically small—cause for celebration indeed, since of those patients who are favored, by the blithely cruel God of Random Chance, with my vanishingly rare cancer, 70 percent experience a recurrence. And virtually all of them are killed by it. This thing is a slate-wiper.
I’m a statistical outlier, incalculably indebted to the man who saved my life by cutting out every last vestige of this murderous thing.
Snaking from mid-belly down to just above my pubic bone, a scar marks the spot where doctors have unzipped my abdomen three times. Sometimes, looking at it in the bathroom mirror, a train track of parallel nubs where the sutures used to be, I’m back in the grayscale limbo of hospital life.
Despite their half-hearted attempts at cheer—paint-by-number seascapes, insistently bright abstracts—hospitals tend toward an institutional grimness: walls painted drab shades of mustard yellow, slate gray, terra-cotta brown; baseboards scuffed by the wheels of numberless gurneys; linoleum faded by countless scrubbings. Even the light slanting in through the windows seems wan, drained of all radiance, as if it had undergone a bloodletting measured in lumens. And then there’s the smell: the ever-present ammonia scent of all-purpose cleaner and underneath it a faint but distinct whiff of cabbage-y rottenness, a bouquet of feces and flatulence and unwashed bodies.
Hospitals aren’t like prisons; they are prisons. True, they’re kinder, gentler ones, whose inmates are usually desperate to be admitted, but even the most grateful patient realizes, at some point, that hospitalization is just a more benign incarceration: the lookalike cell and inevitable cellmate; the swill-bucket food; the patient’s powerlessness in the face of the lowliest flunky; his Kafkaesque uncertainty about when and at whose whim he will be transferred from one hospital to another, or sent to the O.R., or discharged to walk the streets as a free man.
Even the standard-issue hospital gowns and pajama bottoms, generic as prison jumpsuits, encourage a carceral state of mind. Designed to demoralize, the user-unfriendly gowns are slit down the back and ineffectually secured with ties, making them virtually impossible to tie without assistance. With their resemblance to housedresses, they make the male patient feel vaguely transvestic; at the same time, their slit backs remind those of us with a morbid streak of the funeral suits reportedly worn by Dear Departeds to their open-casket viewings. The pants are equally dispiriting: held up by the ubiquitous knotted ties, they’re forever threatening to come undone and expose the sufferer’s bare behind—a constant reminder of the patient’s infantile dependence on nurses, nurse’s aides, or anyone luckless enough to be within earshot when he bleats for help.
The fluorescent purgatory of hospital days can feel like Sartre’s No Exit, staged as an episode of the medical drama House. Around every corner, a Diane Arbus photo come to life: a man sitting alone, on the edge of his bed, holding his penis in one hand, staring at it disconsolately; the immensely fat woman in the room next to mine, spread out on her bed like a blood pudding, bawling melodramatically at the merest needle prick; the family crowded into the room across the corridor, discussing with hale-fellow-well-met heartiness the frequency, laboriousness, and specific gravity of Dad’s bowel movements.
I remember the nurse who hung a bag of potassium on my IV stand, set the drip speed on high, and left the room; the pain was unutterable, the chemical searing my veins like an electrical fire tearing through wiring. I remember waking up in the small hours, beddings soaked through by cold ooze leaking from the surgical drain in my abdomen. I remember the impotent desperation of punching the call button again and again, frantic to rouse a nurse, powerless to help myself in even the smallest of ways. In these waking nightmares, it’s always three A.M., because in the “real dark night of the soul,” as F. Scott Fitzgerald notes, “it is always three o’ clock in the morning.”4 And the nurse never comes.
Recovering from major surgery, we’re helpless as newborns or nonagenarians, moved to tears by the kindness of strangers—or their casual cruelties. Some nurses are candidates for canonization; some missed their calling at Guantanamo. The night after my cancer surgery, I swam up to consciousness, in intensive care, woken by a woman screaming that her oxygen tubes had come loose, that she couldn’t breathe… She screamed and screamed, her voice rising to a ragged crescendo of terror. When no one came, other voices joined hers. A mass of punctures and pain, held together by sutures and butterfly stitches and Foley catheters, I added my hoarse yelp to the chorus of wails coming from nearby beds; every time I yelled, I felt something tearing inside. In the fullness of time, a nurse materialized and, with the dead-eyed unconcern of sleep deprivation and empathy burn-out, plugged the woman’s oxygen tubes into her nostrils.
Yet other nurses were ministering angels, changing my dressings and bringing me ice chips to suck on and tossing me throwaway kindnesses that, in the purgatorial grayness of a hospital day, felt like salvation.
In Illness as Metaphor, Susan Sontag argues that our metaphors come with hidden ideological costs and psychological surcharges that too often blind us to the flesh-and-blood facts of the disease in question. “The most truthful way of regarding illness—and the healthiest way of being ill,” she advises, “is one most purified of, most resistant to, metaphoric thinking.”5 Sontag’s prescription seems especially apt when we consider that illness and injury drag us down, out of the symbolic realm, into the prison of the literal. They reduce us to bodies to be X-rayed, MRI’d, CAT-scanned, intubated, IV’d, woken throughout the night by nurse’s aides armed with blood cuffs and thermometers, pricked at first light by phlebotomists in search of blood samples, sliced or sawed open in the OR, stapled or sutured up, and, ultimately, spirited back to bed to dream the murky submarine dreams of the anaesthetized.
As Elaine Scarry points out in The Body in Pain, “physical pain—unlike any other state of consciousness—has no referential content. It is not of or for anything. It is precisely because it takes no object that it, more than any other phenomenon, resists objectification in language.”6 To the mind in the body in the sickbed or on the operating table, the pain that shadows disease and injury doesn’t stand for anything; it’s experienced as an irreducible sensation, the furthest thing from a figure of speech.
Disease drives a wedge between mind and body, widening the Cartesian split. We’re reminded, with a jolt, that even those of us who live in our heads are alarmingly dependent on the fragile, failure-prone bodies we’d previously regarded as an afterthought. We’re troubled, too, by the wild surmise that the body is Other, an alien thing with a mindless mind of its own.
This is especially so with cancer, a creeping horror that colonizes our bodies one cell at a time, insidiously turning us into It. The philosopher Derek Parfit’s thought experiment comes to mind. Inquiring into the nature of the self, Parfit imagined the science-fictional replacement of your cells, “one by one, with those of Greta Garbo at the age of 30. At the beginning of the experiment, the recipient of the cells would clearly be you, and at the end it would clearly be Garbo, but what about in the middle? […] A self, it seems, is not all or nothing, but the sort of thing that there can be more or less of.”7 Isn’t this what cancer does—turn our bodies, by degrees, into something far less appealing than Garbo, and far more alien?
But even mechanical breakdowns—a small-bowel obstruction, for instance—invite anxious speculation about an Enemy Within. Despite Freud’s dethroning of the conscious mind and the recent assault, by philosophers such as Daniel Dennett, on the very idea of the self, most of us muddle gamely along, confident in the assumption that a homunculus in our heads is still running the show. Disease unsettles that confidence.
When my most recent intestinal blockage sent me to the hospital for 20 nightmarish days, 18 of them without food or water, I struggled to digest the unpalatable fact that I—that is, the thinking, speaking self I regard as the essence of who I am—was at the mercy of my bowel, a brainless but seemingly willful thing that could send me to the ER, doubled over by peristaltic waves of pain, anytime it wanted to.
Of course, your intestines can’t want anything; attributing volition to your innards takes anthropomorphism to certifiable extremes. Nonetheless, metaphors are the skeleton key to a society’s unconscious. It must mean something, at an evolutionary juncture when we seem to be leaving the body behind—hunched over a computer keyboard or diddling a cellphone while our wandering minds are elsewhere, watching video on demand or socializing through screens—that doctors speak in terms of “irritable” bowels, of bowels that “resent” being handled in the OR, of bowels that are “confused” by the dormant period brought on by obstructions and must be “woken up” with stool softeners and bulk fiber supplements and Milk of Magnesia.
Drifting in a Benadryl haze one hospital night, I remembered an article on the enteric nervous system, a network of neurons in our intestines, incapable of conscious thought but complex enough to play a role in our state of mind—a “second brain,” neurogastroenterologists call it, a sobriquet worthy of a 1950s’ creature feature.8 Of course, Dr. Michael Gershon reassures, “The second brain doesn’t help with the great thought processes…religion, philosophy, and poetry [are] left to the brain in the head.”9 Dr. Gershon, who chairs the Department of Anatomy and Cell Biology at New York–Presbyterian, is the author of The Second Brain, whose cover bears a tagline worthy of Ed Wood: “Your gut has a mind of its own.” (Might I suggest, for the revised edition, It Came From Within?) Alone with my night terrors, I worried, Does the good doctor protest too much? In a chapter luridly titled “The Bad Bowel,” in a section called “The Gut is Not Immune to Mental Disease,” Gershon asserts that there is nothing “to prevent the enteric nervous system…from giving rise to enteric misbehavior, independently of any influence the second brain receives from the first.”10 I couldn’t help wondering, Are my entrails, lately the focus of most of my waking thoughts, mounting an insurgency on my brain?
Recovering from surgery, I gaze away long stretches of the day, mind empty as the slate-gray blankness of the Hudson. Hurricane Irene came this way a few days ago, but the river is barely ruffled; it looks almost motionless. The sky is an intense, rain-washed blue. The midday sun is radiant. Or does the world just look supersaturated, from a hospital room?
One thing is certain: the world goes bustlingly on, oblivious to the hungry ghosts in the windows high above. I glimpse cyclists, joggers, rollerbladers on the path that hugs the river, merrily unaware of how lucky they are to be of sound body, alive in the sun, instead of languishing in this morgue for the unwell. Unbidden, a thought whispers in my mind like a ventriloquist’s voice. I hate the living, I hear myself think.
Illness may not be metaphor, but metaphor is the mill we use to grind meaning; it keeps insinuating itself (as it just did) into the stories we tell ourselves about our diseases: Why me? What does it all mean? Even Sontag can’t resist beginning her critique of the cultural costs of metaphor with a metaphor:
Illness is the night-side of life, a more onerous citizenship. Everyone who is born holds dual citizenship, in the kingdom of the well and in the kingdom of the sick. Although we all prefer to use only the good passport, sooner or later each of us is obliged, at least for a spell, to identify ourselves as citizens of that other place.11
The image of sickness as a Limbo of the Lost to which anyone may, without warning, be consigned is a popular one. “Disease has a land, a mappable territory, a subterranean but secure place where its kinships and its consequences are formed,” Foucault writes, in The Birth of the Clinic.12 Christopher Hitchens referred to his transformation from hard-drinking, chain-smoking terror of the debating circuit into cancer sufferer as a “deportation” from “the country of the well across the stark frontier that marks off the land of malady,” a land he called “Tumorville.”13 Elaine Scarry suggests that someone else’s pain—“the events happening within the interior of that person’s body”—“seem to have the remote character of some deep subterranean fact, belonging to an invisible geography that, however portentous, has no reality because it has not yet manifested itself on the visible surface of the earth.”14 Of course, Shakespeare got there first when he rendered death as “the undiscovered country from whose bourn/ no traveller returns.” (Not that death and illness are synonymous, but as Will Self notes in his essay on being diagnosed with a rare blood disease, death is the metaphor we inevitably reach for when we’re ailing, because “when we are ill, do we not always feel like we are dying, even if it’s only a little?”)15
What those who’ve never spent a day in the hospital want to ask those of us who’ve been to the kingdom of the sick and back—or would want to ask, if it ever occurred to the average boomer that he may not die on his rollerblades or midway through the tasting menu—is: What did your trip to the night-side of life teach you? How did it change you? What does it mean to live with the knowledge that you might someday be snatched back into that underworld? All of which is to say: What’s the meaning of malady?
Every patient has his answer. Mine is the existentialist’s koan: the answer is that there is no answer. My first impulse, as a godless rationalist, is to say that diseases like urethral cancer and system breakdowns like bowel obstructions are object lessons in the capriciousness of the cosmos—the unpredictability of life, its random unfairnesses. Our insistence that things have meanings and morals impels us to turn our sickness into metaphor and narrative; to demand something deeper from it than purposeless pain. To my Christian-fundamentalist relatives, my near-fatal cancer was just the Lord moving in mysterious ways, showing me the error of my atheism before death consigned me to eternal torment. To my father, the colorectal cancer that killed him was, he confided in all seriousness, the likely result of a lifetime of emotional repression—karmic retribution for anal retention.
In truth, cancer is a lightning strike out of the godless blue (smokers and workers exposed to environmental carcinogens being the obvious exceptions). Its etiology is often obscure or dauntingly multifactoral. Inspirational tales of sufferers mounting hard-fought “battles” against the Big C aside, a patient’s only active role in his treatment typically consists of choosing an “in-network provider”—a doctor sanctioned by his health insurance—and hoping or praying, as the case may be, for delivery from evil.
To be sure, there are inexhaustibly driven, impossibly resourceful patients like Germaine Berne, the “vivacious psychologist from Atlanta” with a rare and ravenous cancer described by Dr. Siddhartha Mukherjee in his book The Emperor of All Maladies: A Biography of Cancer.
Germaine fought cancer obsessively, cannily, desperately, fiercely, madly, brilliantly, and zealously… Her quest for a cure had taken her on a strange and limitless journey, through Internet blogs and teaching hospitals, chemotherapy and clinical trials halfway across the country… She had deployed every morsel of energy to the quest, mobilizing and remobilizing the last dregs of her courage, summoning her will and wit and imagination…16
But few of us are Germaine Bernes. In the first flush of my cancer diagnosis, I, too, scoured the Web for information, poring over medical journals and newspaper science pages and NIH and CDC FAQs and online forums noisy with the desperate chatter of cancer sufferers. I, too, came to my appointments well-armed with questions, as I imagine Bernes did, interrogating my doctors with prosecutorial zeal. An archaeological dig into my file cabinet turns up the spiral-bound notebook my wife and I took to those early meetings with Dr. McKiernan, head-spinningly intense sessions that left us woozy with information vertigo. Leafing through the pocket-sized book, I come across methodically numbered To Do lists (“opinion of second opinions?”), medical terms to be looked up (“corpora cavernosa”), pop-psych homilies (“depression is normal”), demands for the quantification of the unquantifiable (“How much is chemo going to help me? 5 percent? 95 percent?”), a laconic note acknowledging the worst-case scenario without comment (“if it [my cancer] comes back, incurable”).
Soon enough, however, I was defeated by the Herculean labors demanded of the amateur cancer researcher. Hacking my way through a thicket of medical jargon was a thankless task that became exponentially more thankless when the thicket turned out to conceal just how little medical science knows about 40-something men with my obscure cancer, which typically targets geriatric women. Most of all, though, I simply didn’t want to allow the disease to metastasize across my mind, occupying my thoughts as it already had my body.
Yet, looking back on My Cancer Year, it occurs to me that perhaps we do bring something back from the land of malady—not a meaning or moral in the capital-“M” sense, necessarily, but maybe a philosophical memento, some little insight that, in a kind of existential parallax effect, subtly shifts our perspective on everyday life.
For me, that insight is the grudging admission that there’s some truth in the notion that serious illness is a touchstone, revealing the stuff we’re made of. Hitchens’s unbowed atheism in the face of a cancer so rapacious only five percent survive it is unquestionably the measure of the man, an inspiring lesson in the consolations of reason in an age of birthers, truthers, anti-vaccination crusaders, global-warming know-nothings, and Darwin-denying god-botherers.17 Likewise, we can see Sontag’s sublimation of her dark passage through breast cancer, in the omniscient historiography of Illness as Metaphor, as a resolute refusal to allow herself to be redefined as a cancer “victim”—a chemo-clouded mind subservient to the needs of the abject flesh.
As a career patient, I’ve learned one thing at least: the importance of clinging to the rag-end of your sense of self, however you define it—intellect, sense of humor, generosity of spirit, a stoicism worthy of Seneca or Mr. Spock, or, in a writer’s case, the mind that makes sense of itself as a reflection in the mirror of language. In the M.A.S.H.-unit chaos of the E.R.; in the nowhere, notime of the hospital room; in the O.R., where the euphoria of oncoming anesthesia and the doting attentions of apparitions in scrubs make you understand, in an instant, the perverse seductions of Munchausen’s Syndrome as you ride into the stage-light radiance on your gurney like the Son of Heaven in his sedan chair, feeling for all the world like a pathological celebrity—in these moments of inescapable embodiment, I’ve learned to float free in my head, a thought balloon untethered from the body on the sickbed or the operating table.
In The Body in Pain, Scarry contends that “physical pain has no voice”; that its profoundly subjective nature confers on it an “unsharability” that makes it fundamentally resistant to linguistic expression. “Physical pain does not simply resist language but actively destroys it,” she argues, “bringing about an immediate reversion to a state anterior to language, to the sounds and cries a human being makes before language is learned.”18 I contend that, while metaphor may be an illness when it obscures our understanding of the true nature of disease, language—the meta-metaphor—is the Indian rope trick that lets us climb into our minds, out of bodies in pain.
Propped in a lawnchair in my backyard after weeks entombed in a hospital room, I think of Hitchens’s remark to an interviewer, shortly after learning he had metastasizing esophageal cancer. “I was very afraid it would stop me writing,” he said. “And I was really petrified with fear about that because I thought that would, among other things, diminish my will to live because being a writer’s what I am rather than what I do.”19
I am a story narrating itself into being, I think. A strange loop of mind and language—the ontological equivalent of “Drawing Hands,” a picture by M.C. Escher of a right hand drawing the left hand that is drawing the right. It may be true, as the linguist Steven Pinker maintains, that the human capacity for language is an evolutionary adaptation. But language, in turn, shapes the internal monologue that narrates the conscious self into existence. The I that says “I” is the only I; the self is a center of narrative gravity.20
Drawing Hands, M.C. Escher. Lithograph, 1948.
© Cordon Art-Baarn-the Netherlands.
Through closed eyes, I sneak a glance at the sun; a fireball flares across my lids. I’ve read the surgeons’ “operative notes” on my surgeries, read them as if they were postcards chronicling a trip taken in another lifetime, to a country whose name has changed so many times and whose borders have been so repeatedly redrawn that it can’t be found on any map. My nine-hour cancer surgery: “The patient was administered general endotracheal anesthesia and placed in the dorsal lithotomy position, prepped and draped in the usual sterile fashion. … An incision was made in the perineum…” My most recent bowel-obstruction surgery: “Exploration was performed with the findings of abdominal cocoon [a fibrous membrane of surgical scar tissue swaddling the bowel]. The adhesions were carefully taken down using sharp and blunt dissection.” Reading these travelogues from the dark interior makes me feel like Lazarus, post-traumatically stressed by memories of what it’s like to die and rise again.
I was the body lying on the table, prepped and draped in the usual sterile fashion, tumors and adhesions carefully taken down using sharp and blunt dissection; I am the body sitting in the sun, passing for healthy and whole. I shift slightly, tracking the light as it moves across the yard. On one arm, a grayish blotch tattoos the spot where surgical tape secured an IV, the tenacious adhesive resistant to weeks of showers and scrubbings. Through my shirt, I can feel the rubbery seam of the “midline incision” created by my first surgery, a souvenir of a trip that took me perilously close to the border of the undiscovered country whose visitors never return.
“I’m alive,” I say, out loud. More than the sound of my voice, it’s the way language gives thought a body—the shape and weight of words, like smooth stones in the palm of the mind—that makes me believe it.
— Mark Dery
© Mark Dery; all rights reserved. No part of this work may be reproduced, except under Fair Use provision of U.S. copyright law, without author’s written permission. Author contact: markdery AT markdery DOT com.
Design: Rob Beschizza
1 This illustration is taken from the “Faces Pain Scale Revised (FPS-R)” page of the Geriatric Pain Website, developed by Sigma Theta Tau International for the Center for Nursing Excellence in Long Term Care, Link.
2 “Faces Pain Scale Revised (FPS-R),” accompanying text, Geriatric Pain Website, Link.
3 Mark Dery, “Cancer-Gram #2,” mass e-mail from the author to friends and family, September 26, 2006, 5:41 P.M.
4 F. Scott Fitzgerald, “The Crack-Up” in The Crack-Up (New York: New Directions, 2009), p. 75.
5 Susan Sontag, Illness as Metaphor (New York: Farrar, Straus and Giroux, 1978), p. TK.
6 Elaine Scarry, The Body in Pain: The Making and Unmaking of the World (New York: Oxford University Press, 1985), p. 5.
7 Larissa MacFarquhar, “How to Be Good: An Oxford philosopher thinks he can distill all morality into a formula. Is he right?,” The New Yorker, September 5, 2011, p. 43.
8 Adam Hadhazy, “Think Twice: How the Gut’s ‘Second Brain’ Influences Mood and Well-Being,” Scientific American, February 12, 2010, Link.
9 Quoted in Hadhazy, “Think Twice,” Scientific American, ibid.
10 Michael D. Gershon, The Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and Intestine (New York: HarperPerennial, 1999), p. 177.
11 Susan Sontag, Illness as Metaphor, p. 3.
12 Michel Foucault, The Birth of the Clinic: An Archaeology of Medical Perception (New York: Vintage Books, 1975), p. 149.
13 Christopher Hitchens, “Topic of Cancer,” Vanity Fair, September 2010, Link.
14 Elaine Scarry, The Body in Pain, p. 3.
15 Will Self, “The Trouble with My Blood,” The Guardian, October 21, 2011, Link.
16 Siddhartha Mukherjee, The Emperor of All Maladies: A Biography of Cancer (New York: Scribner, 2010), p. 470.
17 “Only five percent survive it”: See transcript of 60 Minutes interview with correspondent Steve Kroft, “Outspoken and outrageous: Christopher Hitchens,” March 6, 2011, 10:22 P.M., Link.
18 Elaine Scarry. The Body in Pain, p. 4.
19 Quoted in “Outspoken and outrageous: Christopher Hitchens,” ibid.
20 Daniel Dennett, “The Self as a Center of Narrative Gravity” in F. Kessel, P. Cole and D. Johnson, eds, Self and Consciousness: Multiple Perspectives (Hillsdale, NJ: Erlbaum, 1992), Link.
Buy Mark Dery’s new book
I Must Not Think Bad Thoughts: Drive-by Essays on American Dread, American Dreams
Read more at Boing Boing: Health &
Books